Human Reproduction
1. The Male Reproductive System
2. The Female Reproductive System
3. Gametogenesis
4. Menstrual Cycle
5. Fertilisation and Implantation
6. Pregnancy and Embryonic Development
7. Parturition and Lactation
The chapter on Human Reproduction in Class 12 Biology is a comprehensive exploration of the reproductive processes in humans. It covers the anatomy and functions of the male and female reproductive systems, the process of gametogenesis, the intricacies of fertilization, and the subsequent stages of pregnancy. The chapter also discusses reproductive health and its significance for overall well-being.
Here are a key points and Detailed Notes from the chapter:
Human Reproduction
1. THE MALE REPRODUCTIVE SYSTEM
Human male reproductive system consists of:
○ The primary sex organs, i.e., a pair of testes.
○ The secondary sex organs i.e., the duct system
and associated glands and
○ External genitalia
Diagrammatic sectional view of male pelvis
showing reproductive system
Testis
- Located outside the abdominal cavity (extra abdominal) with in a pouch called scrotum; scrotum provides a temperature 2.0 – 2.5°C lower than the body temperature necessary for spermatogenesis.
- Each testis is oval in shape and measure about 4 to 5 cm in length, 2–3 cm in width and about 3 cm in thickness.
- The testis is covered by a dense covering called tunica albuginea.
- Internally the testis is divided into about 250 compartments, called testicular lobules.
- Each lobule contains 1–3 highly coiled seminiferous tubules (the structural and functional units of testis) in which sperms are produced.
- The seminiferous tubule has a tunic of connective tissue and is internally lined by seminiferous or germinal epithelium.
- The seminiferous epithelium consists of two types of cells: (1) Sertoli cells and (2) spermatogonia, that form the male germ cells or spermatozoa.
- Sertoli cell provide nutrition and shape to the developing germ cells and spermatozoa.
- The spermatogonia undergo cell divisions to form spermatozoa.
- The spaces called interstitial spaces, between the seminiferous tubules have connective tissue, which includes blood vessels and Leydig cells (also called Interstitial cells); Leydig cells synthesise and secrete the male sex hormones called androgens of which testosterone is the principal one.
Duct System
- The intratesticular duct system starts with tubuli refti, which are the short and straight end segments of the seminiferous tubules; these tubles open into vasa efferentia, through rete testis.
- Vasa efferentia conduct the sperms out from the testis and open into the epididymis.
- Epididymis is a single convoluted tubule that is located along the posterior surface of the testis.
- The epididymis continues as the vas deferens that ascends into the abdominal or pelvic cavity through inguinal canal.
- It loops over the urinary bladder and receives a duct from the seminal vesicle (of its side) to form ejaculatory duct that runs through the prostate and opened into the prostatic urethra, just after its other gene from the urinary bladder.
- The urethra receives the ducts of prostate gland and the bulbourethral (Cowper’s) glands a little ahead and runs through the penis to its external opening; called urethral meatus.
Accessory Glands
- The accessory glands of male reproductive system include:
○ a pair of seminal vesicles,
○ a prostate gland and
○ a pair of bulbourethral glands (also called Cowper’s glands)
- Their secretions are collectively called as seminal plasma.
- Seminal plasma is rich fructose, calcium, and certain enzymes; it provides nutrition and a medium for the spermatozoa to swim in the female reproductive tract.
- The seminal plasma along with the spermatozoa, is called semen.
External Genitalia
- Penis is the external genitalia in human males.
- It is made up of special erectile tissue, that helps in erection of the penis to facilitate insemination.
- The enlarged tip of the penis is called glans penis; it covered by a loose fold of skin called foreskin of prepuce.
2. THE FEMALE REPRODUCTIVE SYSTEM
Human female reproductive system consists of:
○ The primary sex organ i.e., A pair of ovaries.
○ The secondary sex organs i.e., The duct system consisting of a pair of fallopiantubes, a uterus, cervix and vagina.
○ The external genitalia and
○ Mammary glands
Ovaries
- Ovaries are the primary female sex organs that produce the female gametes (called ova) and secrete the ovarian or sex hormones.
- The ovaries are located in the abdominal/pelvic cavity, one on each side near the kidney.
- Each ovary is an almond-shaped body about 3 cm long, 1.5 cm broad and 1 cm thick.
- It is attached to the pelvic wall and uterus by ligaments.
- The ovary is covered by a thin epithelium, which encloses the ovarian stroma.
- The stroma is divided into two regions: (1) a peripheral cortex and (2) and inner medulla.
- The ovarian follicles are found in various stages of development in the cortex.
The Duct System
Fallopian Tube
- A fallopian tube extends from the periphery of each ovary to the uterus; it is a muscular tube of about 10–12 cm long situated above and behind the urinary bladder.
- The part of fallopian tube closer to the ovary is funnel-shaped and is called infundibulum.
- The edges of the infundibulum possess fingerlike projections, called fimbriae, that help in collecting the ovum during ovulation.
- The infundibulum leads into a wider part of the fallopian tube or oviduct, called ampulla.
- The last part of the fallopian tube that joins the uterus is narrow and it is called isthmus.
Uterus
- It is an inverted pear-shaped muscular structure, attached to the pelvic wall and supported by ligaments.
- The wall of the uterus has three layers of tissues.
- The outermost or external layer is the thin, membranous perimetrium.
- The middle thick layer of smooth muscles is called myometrium.
- The innermost glandular layer is endometrium, which lines the uterine cavity.
- The contractions of the smooth muscles of the myometrium are responsible for the expulsion of the baby during parturition.
- The endometrium undergoes cyclic changes during menstrual cycle.
- The uterus opens into the vagina through a narrow cervix.
Vagina
- It is a muscular tube-like structure that opens to the outside.
- The vagina is partially covered by a membrane called hymen.
- The cervix and the vagina together constitute the birth canal.
- The functions of vagina are to
○ receive the male gametes during insemination.
○ serve as the birth canal during parturition.
External Genitalia
- The female external genitalia include:
○ mons pubis
○ Labia majora
○ Labia minora
○ Clitoris
○ Hymen
- Mons pubis is a cushion-like fatty tissue covered by skin and pubic hair.
- It extends down as a pair of fleshy folds of tissue, called labia majora and surround the vaginal opening.
- The labia minora are paired folds of tissue under the labia majora; it also surrounds the vaginal opening.
- The labia minora enclose a space posteriorly, called vestibulum and anteriorly unite and form a conical projection, called clitoris, above the urethral opening.
- Hymen is the membrane that partially covers the vaginal opening; it becomes ruptured due to vigorous physical activities or during the first coitus.
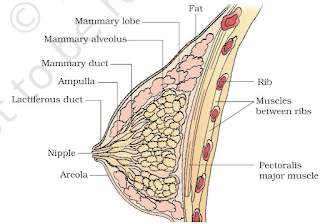
Mammary Glands
- A human female has a pair of functional mammary glands that consist of glandular tissues and variable quantity of fat.
- The glandular tissue is divided into 15–20 mammary lobes; each lobe contains clusters of cells, called alveoli, which open into mammary tubules.
- The mammary tubules of each lobe join to form a mammary duct.
- Several mammary ducts join to form a wider mammary ampulla that is connected to lactiferous duct, through which milk comes out.
- The milk is actually secreted by the cell of alveoli and is stored in the lumen of alveoli.
3. GAMETOGENESIS
The primary sex organs – the testis in the males and the ovaries in the females – produce gametes, i.e, sperms and ovum, respectively, by the process called gametogenesis.
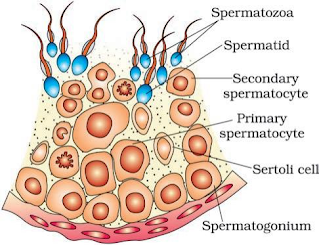
Spermatogenesis
- It is the process of formation of spermatozoa in the testis; the process starts at puberty.
- The spermatogonial cells present on the inner wall of semiferous tubule multiply by mitotic division.
- Some of the spermatogonia serve as stem cells for spermatogenic lineage.
- Other spermatogonia function as progenitor cells or the precursors of spermatozoa.
- They undergo changes by accumulating food materials and grow almost double in size and become the primary spermatocytes.
- Each primary spermatocyte undergoes the first meiotic division and forms two haploid secondary spermatocytes.
- The secondary spermatocytes undergo the second meiotic division leading to the formation four equal sized, haploid spermatids.
- The spermatids are transformed into spermatozoa by process of spermiogenesis.
- The sperm heads become embedded in the Sertoli cells and are ultimately released from the seminiferous tubules by the process of spermiation.
Hormonal Control of Spermatogenesis
- Spermatogenesis is initiated due to an increase in the secretion of gonadotropin-releasing hormone (GnRH) by the hypothalamus at the age of puberty.
- The increased level of GnRH act on the anterior pituitary and stimulate the secretion of two gonadotropins, i.e., luteinizing hormone (LH) and follicle stimulating hormone (FSH).
- LH acts on the Leydig cells and stimulates them to secrete testosterone.
- FSH acts on the Sertoli cells and stimulates secretion of some factors, which help in spermiogenesis
Structure of a Spermatozoan
- The whole body of a spermatozoan is enveloped by a plasma membrane.
- A human sperm is composed of four parts; heat, neck, middle piece and tail.
Head
- Head contain an elongated, compact, haploid nucleus, i.e., concentrated DNA.
- The anterior end has a cap-like structure, called acrosome; the acrosome contains enzymes that helps in dissolving membranes of the ovum for fertilization.
Neck
- Neck contains two centrioles, a maximal centriole, which is necessary for the first cleavage division of zygote and a distal centriole, that is connected to the tail filament.
Middle Piece
- Middle piece contains a number of mitochondria, that provide energy for the motility of sperms.
Tail
- It consists of an axial filament surrounded by the plasma membrane.
- It helps the sperm to move in the female reproductive tract towards the female gamete (ovum) for fertilization.
Oogenesis
- Oogenesis is the process of formation of female gametes or ova in the ovary.
- Oogenesis is initiated during embryonic development in a female foetus.
- All the oogonia (about a million) are formed in the ovary of the foetus of 25 weeks; no new oogonia are formed after birth.
- The oogonial cells which enter meiosis I, are the primary oocytes but the division remains suspended in prophase I; other cells form the granulosa/follicle cells and forego the potential of forming ova.
- The primary oocyte becomes surrounded by a layer of granulosa cells and is called the primary follicle.
- A large number of these follicle degenerate before puberty (follicular atresia) and only about 60000 – 80000 are left in the ovary.
- The primary follicles become surrounded by more layers of granulosa cells and a thecal layer; at this stage they are called secondary follicles.
- As development continues, a cavity develops in the secondary follicle around the primary oocyte; it is called antrum and is filled with a fluid called, liquor folliculin.
- Simultaneously, the thecal layer becomes organized into an outer theca externa and at this stage the structure, is called tertiary follicle.
- As the tertiary follicle continues its development, the primary oocyte completes its meiosis I and forms a large-cells, the secondary oocyte and a tiny cell, first polar body
- The secondary oocyte grows in size with a bulk of nutrient-rich cytoplasm.
- The tertiary follicle becomes changed into a mature follicle, called Graafian follicle.
- The secondary oocyte forms a new membrane, called zona pellucida, around it.
- The secondary oocyte starts its second meiotic division, but it is suspended in metaphase II, until a sperm enters it.
- At this stage, the Graafian follicle ruptures to release the secondary oocyte form the ovary.
4. MENSTRUAL CYCLE
- The cyclic changes that occur in the reproductive organs of primate females (monkeys, apes and human beings), constitute the menstrual cycle.
- The cycle of events starts from one menstruation till the onset of the next and lasts for about 28/29 days (a mensem).
- The beginning of menstruation at puberty, is called menarche.
- One ovum is released during the middle of each menstrual cycle.
- The events in a menstrual cycle can be studied under four phases:
Menstrual phase
- The cycle starts with this phase and the menstrual flow (menstruation) lasts for 3–5 days.
- It results due to the breakdown of endometrial lining of the uterus and its blood vessels, along with the unfertilized ovum.
Follicular phase or Proliferative Phase
- In this phase, the primary follicles in the ovary grow and become a fully mature Graafian follicle.
- The endometrium of the uterus is regenerated by proliferation of its cells.
- These changes are due to an increased level of pituitary hormones, FSH and LH and ovarian hormone, estrogen.
- FSH controls the follicular phase; it stimulates the growth of follicles and secretion of estrogen by the growing follicles.
- Both FSH and LH reach their peak level in the middle of the cycle (about 14th day)
Ovulatory Phase
- The peak level of LH (called LH surge) induces the rupture of the mature Graafian follicle and thereby the release of ovum; this process is called ovulation.
Luteal phase/Secretory Phase
- During this phase, the ruptured follicle is transformed into corpus luteum.
- It secretes large quantities of progesterone, needed to maintain the endometrium.
- The endometrium thickens further and their glands secrete a fluid into the uterus.
- In the absence of fertilisation, corpus luteum degenerates and this causes disintegration of the endometrium leading to menstruation
- The menstrual cycles cease at the age of about 45–50 years; it is called menopause.
5. FERTILISATION AND IMPLANTATION
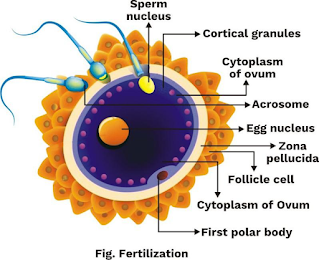
Fertilisation
- During copulation, the semen is released by the penis into the vagina; this process is called insemination.
- The motile sperms move through the cervix, enter the uterus and reach the ampullary-isthmic junction of the fallopian tube.
- The ovum released from the ovary also reaches the ampullary-isthmic junction, where fertilization takes place.
- As sperm comes in contact with the zona pellucida layer of the ovum and induces changes in the
- membrane to block entry of other sperms; thus, only one sperm can enter an ovum(secondary oocyte).
- The enzymes of the acrosome of sperm help to dissolve zona pellucida and plasma membrane of the ovum for the entry of the sperm into the cytoplasm of the ovum (secondary oocyte).
- The entry of sperm induces the completion of second meiotic division of the secondary oocyte, that results in the formation of a haploid ootid and a small second polar body.
- Even before the nucleus of the ootid is organised, it fuses with the sperm nucleus (fertilization) to form a diploid zygote.
Development of Zygote
Cleavage
- The zygote undergoes successive (mitotic) division, called cleavage, as it moves through the isthmus of fallopian tube towards the uterus.
- The daughter cells are called blastomeres.
Morula
- The embryo with 8 to 16 blastomeres, is called morula; at this stage it is a solid sphere.
Blastocyst
- Cell divisions continue in the morula and the blastomeres become arranged along the periphery leaving a central cavity, called blastocoel; the embryo at this stage, is called a blastocyst.
- The cells now become arranged as an outer layer, called trophoblast and an inner group of cells, called inner cells mass, that is attached to trophoblast and projecting into the blastocoel.
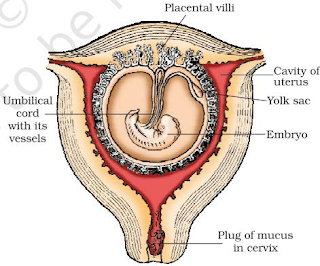
Implantation and Placenta Formation
- The trophoblast layer gets attached to the endometrium.
- The cells of endometrium divide rapidly and cover the blastocyst.
- So, the blastocyst gets embedded in the endometrium; this process is called implantation; it leads to pregnancy.
- After implantation, finger-like projection, called chorionic villi appear from the trophoblast; they are surrounded by the uterine tissue and material blood vessels.
- The chorionic villi and the uterine tissue become interdigitated to form placenta, the structural and functional unit, between the foetus/embryo and the uterine wall of the mother.
- Umbilical cord, the structure that connects the placenta with the foetus, helps in transport of substances to and from the foetus.
- Placenta performs the following functions:
○ It facilitates supply of oxygen and nutrients to the foetus.
○ It also helps in the removal of carbon dioxide and other excretory products from the foetus.
○ It acts as an endocrine tissue and secretes and following hormones:
- human chorionic gonadotropin (hCG)
- human placental lactogen (hPL)
- progestogens and
- estrogens; these are necessary for the foetal growth and maintenance of pregnancy.
- The levels of other hormones like estrogens, progestogens, control, prolactin, thyroxine, etc also increase several-folds in the material blood.
6. PREGNANCY AND EMBRYONIC DEVELOPMENT
- Simultaneous with the development of placenta, the inner cell mass differentiates into an outer layer, called ectoderm, and an inner layer, called endoderm.
- A middle layer, called mesoderm appears between the ectoderm and endoderm.
- These primary germ layers give rise to all the tissues and organs of the adult.
- After one month of pregnancy, the heart is formed; the first sign of growing foetus is the heartbeat.
- By the end of second month, the foetus develops limbs and digits.
- By the end of third month (first trimester) most of the organ systems are formed.
- During the fifth month eruption of hair on the head is observed; the foetus also shows movement.
- By the end of six month (second trimester) the body is covered with fine hair, eyelids separate and eyelashes are also formed.
- By the end of eight month of pregnancy, the tests (in case of a male foetus) descend into the stratum.
- By the end of nine months of pregnancy, the foetus is completely developed and is ready for its delivery.
-
Ovary secretes a hormone, called relaxin towards the end of pregnancy.
7.PARTURITION AND LACTATION
Parturition
- The average duration of pregnancy (gestation period) is about nine months.
- The ovary at this period secretes a hormone, called relaxin, that facilities parturition by softening the connective tissue of symphysis pubica.
- Parturition is induced by a complex neuroendocrine mechanism that involves cortisol, estrogens and oxytocin.
- The signals for parturition arise from the fullydeveloped foetus and the placenta; they induce mild uterine contractions, called foetal ejection reflex, which triggers the release of oxytocin from the posterior pituitary of the mother.
- Oxytocin acts on the uterine muscles and causes stronger uterine contractions, which in turn stimulates secretion of more oxytocin.
- The stimulatory reflex between the uterine contraction and oxytocin secretion continues and result in stronger and stronger contraction of uterine muscles, leading to the expulsion of the fully-developed foetus (now, the infant) from the uterus through the birth canal, i.e., parturition is achieved.
- It is followed by the expulsion of placenta and the remains of umbilical cord.
Lactation
- The mammary glands also undergo certain development during pregnancy under the influence of hormones like prolactin (hPL) and Progesterone.
- They start producing milk towards the end of pregnancy and the milk is used for feeding the new-born (lactation).
- The milk that comes out of the mammary glands of the mother during the initial few days of lactation, is called colostrum; it contains several antibodies needed to develop resistance in the new-born baby.




















Sir Please sabhi chapter ka aise hi notes upload kar dijiye
ReplyDeleteplzz upload principles of inheritance and variation also
ReplyDeleteit is imp. for my pre_boards and neet also